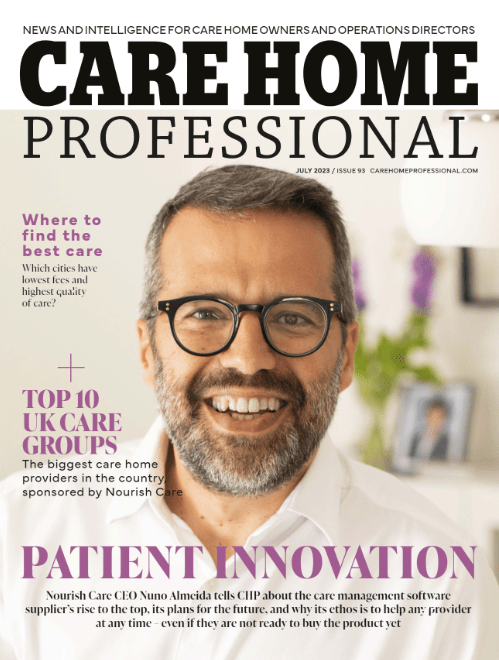
Our founder and CEO, Nuno Almeida, is featured on Care Home Professional’s cover for July 2023.
Nuno shares his thoughts on the social care sector, the growth and future of Nourish and how we align closely with the ambitions of our customers.
“We think we have the best product in the market. What makes the difference is our understanding of how a good digital product – with the right integrations, data science, sector knowledge, when all brought together – can translate into better outcomes for people needing care. We can do this from a single care home to hundreds of locations with a variety of types of care.”
Want to know more about how Nourish can work for you? Book a personalised demo with our team and see how Nourish can truly adapt to your care service.
We all understand the importance of valuing and respecting those we care for, when we speak about how you can truly deliver dignity in care, it might be hard to conjure up an exact idea of what that really means or looks like. Luckily Dignity in Care has come up with the 10 Dignity Do’s – an easy list that describes the values and actions of a high-quality care service that respects and upholds people’s dignity to the highest standard.
A Dignity Champion is a person who believes that being treated with dignity is a basic human right, not an optional extra. They believe that care provision must be: compassionate, person-centred, efficient and effective, and are willing to take action in order to achieve this.
“I have handed out Dignity in Care 10 Point ‘Dignity Do’s’ Cards to all staff in my care home – each time we have a team meeting we focus on one of the 10 Dignity Do’s and discuss what we can do to meet that challenge. Each meeting results in us making changes to the way we provide care.”
– A Dignity Care Champion
Dignity Champions are those in a care organisation that champion and uphold the 10 Dignity Do’s, as well as advocate and share the importance of dignity in any form of care. This includes:
You can find out more about becoming a dignity champion and the 10 Dignity Do’s by visiting Dignity in Care’s becoming a champion or register page. Another helpful resource is the Dignity Champion’s Toolkit for Action, which includes actionable insights, ideas and advice for people in a range of different care roles to help make a difference and bring dignity to care.
There are many ways that the Dignity Do’s can help care groups, teams and organisations improve their level of care and adapt to offer a continuously improving level of service. Championing the Dignity Do’s is only the start, we believe that in order to provide the highest quality care, moving to digital care planning enables you to create personalised care plans, record care accurately at the time of providing care and understand and act on trends about those you care for. By using digital, you can be much more efficient and spend more time providing person-centred, quality care.
To find out how care software and technology can be used to enhance your care service, or help you to better care for those you support, book a demo or get in touch with the team.
Thank you to Warrington Community Living for sharing the following article on their website. We love hearing how Nourish‘s digital platform is helping and improving care services across the country!
We’re all taught that oral health is essential to keep our teeth healthy but what does this really mean? Poor oral health can lead to malnutrition, pneumonia and a weakened immune system which can make it harder to recover from common illnesses. Studies are being conducted to see whether dental hygiene has any links to dementia. So how can we encourage better dental hygiene?
Getting people you support to the dentist is no easy feat. Dental practices aren’t always accessible, medical settings can be quite distressing and getting there requires accessible transport and extra staff. Instead of taking the people you support to the dentist, why not bring the dentist to you? Domiciliary dental services provide dental care right at home.
Some local NHS trusts offer training on dental health for a few members of staff, appointing these staff members as Oral Health Champions. These Champions undertake the training and the responsibility of training existing and new staff. Ensuring your service is working to the NICE guidelines and the Oral Health policy could also become part of the Champions’ role.
Activities are a simple and fun way to encourage conversations about good oral health. Brushing your teeth may not seem fun but, depending on the people you supports abilities, it can be! If you have any keen knitters, download knitting patterns for knitting teeth, tooth fairies or tooth fairy pouches for grandchildren, young relatives and friends’ children. Arty people could have a go at crafting teeth and toothbrushes out of leftover cardboard and painting them. If you have any connections to a local school or nursery, invite them over (Covid-19 permitting) for a lesson on mouthcare. You could even have a sensory afternoon of science experiments, making elephant toothpaste, growing plaque with yeast and sugar and, egg brushing.
The Nourish platform allows dental hygiene to be logged, tracked and managed and provides an Oral Health Assessment Tool (OHAT) for new admissions. In Nourish, you are able to plan, manage and evidence dental appointments and visits and use the OHAT for regular reviews on the oral health of those you support. The Alerts and Warnings function can ensure appointments and reviews are not missed. Because dental health can have a significant impact on the general health of the people you support, the ability to monitor means early intervention is possible.
Many of us use some kind of technology to monitor our health and well-being. We’ve got fitness trackers, smart watches, sleep trackers, fluid logs, gym apps and so much more. We input our data and track our progress so we can see where and how we can make changes to improve our health. And just as it can improve our health, data and analytics can improve your care management too!
With this in mind, the same concept is now being applied in the care sector. Care teams are now able to use a digital system to record notes and assist with daily care. Moving away from a paper-based system comes with a whole host of benefits, one of which is the huge amount of data that can be analysed, which has great potential to improve the way care and support is provided.
In order to look at ways in which care can be improved, measurable data is needed. Not only will this help to spot any initial areas for improvement, but the continuous monitoring of data allows you to accurately measure the effects of any changes made. A data-driven approach to care can really help care teams to better understand those they support, and feel confident they are providing the safest daily care to each individual.
Fears surrounding big data
Although the idea of using data analysis is supposed to instill confidence in carers, it is understandable that many people still have their reservations about this, mainly surrounding the accuracy of said data, and where data protection comes into the equation. But when it comes to the digital vs paper debate, it is clear that paper recording poses a far greater risk for inaccuracy and inconsistencies in patient information.
We are already starting to see technology being implemented within the health and social care sectors. The NHS is slowly starting to work on digitalisation of patient records, and electronic care planning is now becoming the norm across many care homes in the UK. Now that the care sector is rapidly adopting a digital way of working, data analytics is the next step in evolving and enhancing the way we care. But how exactly can data and analytics improve your care management?
Spotting trends in those you support
One of the main benefits of analysing data is to be able to spot trends. This could be anything from eating habits to sleeping patterns, and these trends may vary between care providers.
What this allows carers to do is look at the bigger picture. Did someone refuse their dinner or their medication one night? If so, why did they? Who was on shift that evening? When looking at the bigger picture you can start to see what’s missing or what’s changed and ask the necessary questions to get to the bottom of it.
With paper recording, it can be a little trickier to keep up to date with the bigger picture and see things clearly, meaning things can get missed. While it may sound extreme, spotting someone’s decline in appetite could be the difference between life or death, as this could be the first sign of an underlying condition that could otherwise go unnoticed.
Creating continuity of care
Having data recorded electronically makes it far easier to run reports, and gain insight into individual’s needs. This type of data recording and reporting is proactive and allows you to share insight and information with your care team and other healthcare providers in a safe and efficient way.
With data reports readily available to view, this is a far more accurate way of sending and receiving up to date information, ensuring that everyone is getting the right level of care they require.
Creates a transparent care environment
When there is clear communication among care teams, you are better equipped to support those in your care. Going digital has its benefits in ensuring everyone is on the same page, but the analysis of data takes this one step further.
By providing everyone with the facts and figures in a clear and concise way, these insights will empower carers to be the best they can be. With reports and data readily available, this means everyone can have clarity around the type of care an individual needs and what is being done to support them, and family members can be kept in the loop so they have peace of mind their loved ones are in good hands.
Transparency is key when it comes to evidencing care for CQC purposes. Data analysis better equips you to provide the best quality care as well as have all the necessary information readily available for inspectors when you have an audit.
The future of data and analytics in a post Covid-19 world
This year, the care sector has faced many challenges. The Covid-19 pandemic swept across the globe and sadly became one of the leading causes of deaths within care. Understanding something like this virus can become a lot easier when we’re able to analyse the facts and the figures. Care homes who were successful in preventing an outbreak within their organisation were monitoring things extremely closely. Symptoms, incubation periods, and patient-staff interactions were all recorded and able to be analysed to track and prevent outbreaks from sweeping through their care service.
Data and analytics is quickly going to become a must within the care sector in a post-pandemic world. The Goverment have already invested £600 billion into an Infection Control Fund for care homes, and using that funding for digital transformation could help so many care services become better prepared in the future. Not only does technology make it far easier to breakdown and understand data, but using a digital device to share information with staff, families and other healthcare services is far safer as it reduces contact between one another. Staff will be able to work more efficiently when they can all access a centralised system remotely, and it’ll be easier to log and track who has been where and when which will ultimately help prevent the spread of the virus.
How electronic care planning can help
Moving towards a digital way of working has a number of advantages, and now is the time for care services who are still using paper records to make the switch. Collating and using big data allows care teams to become more aware and vigilant of the risks to those they support, understand those risks, and implement solutions. At Nourish, we want to encourage data analysis to help care organisations provide better care, which is why our electronic care planning system can also be upgraded with an analytics tool that can help spot trends and patterns to better equip you in supporting those in your care.
We now also have a Covid-19 Tracker built into our platform, so you can track the virus more closely and understand how it is affecting your care service. To find out more about how Nourish can help you provide better care, book a demo with us today.
As the Coronavirus pandemic swept the globe and hit the UK earlier in March this year, care homes were put under more strain than they ever have before. Working to ease the pressure on the NHS, many care organisations have and continue to act as an overspill for hospitals when they get too busy. This has meant taking on patients who potentially were still infectious with coronavirus, as demand for beds soared across the UK. We take a look at Coronavirus in care homes, and how care has been managed in cases of Covid-19.
Care teams have felt they’ve been let down by the government, being told they shouldn’t need to work any differently, even once Covid-19 had hit the UK. There has been an overall shortage of PPE (personal protective equipment), but care teams were being told by suppliers that the NHS took priority.
Care homes usually implement what is known as “barrier nursing” when someone contracts a virus. This is where the person is isolated and new gloves, mask, paper towels etc will be used for each and every patient. However, with the realisation that Covid-19 could often be asymptomatic, and without antibody tests readily available, this posed a problem for managing Coronavirus in care homes. Combine that with the sudden influx of patients from the NHS, the lack of PPE stock and such close quarters within care homes, for many it felt like they were set up to fail.
Many care workers have reported full floors of homes being wiped out by this silent killer, leaving staff devastated and terrified for their own safety, too.
The facts and figures of Coronavirus in care homes
On the 15th May 2020 the statistics on Covid-19 related deaths in the UK care sector was released. Between the period of 2nd March and 1st May 2020, there have been 12,526 deaths involving Covid-19, which is said to be 27.3% of all deaths of care home residents.
Coronavirus in care homes was the leading cause of death in male residents and second leading cause of death in women, after Dementia and Alzheimer’s, which was also the main pre-existing condition found amongst Coronavirus deaths.
Figures have been taken from the Office for National Statistics, published on 15th May 2020.
Are outbreaks of Covid-19 inevitable in care homes?
Covid-19 is highly risky for people living with multiple pre-existing conditions, is highly infectious, and many care teams lack the means to closely monitor and track potential symptoms of the virus amongst everyone in their care. By the time the government had addressed the nation on the severity of the coronavirus pandemic, many lives had already been lost as the virus found its way into care settings. It is generally accepted that hospital discharges of untested patients who moved into care homes increased the risk of contracting the virus by other residents.
And in addition to this, self-isolation measures led to sudden staffing shortages, with many homes having no chance but to bring in agency staff, meaning care workers are moving from home to home, once again increasing the risk of transmission.
For the homes that have been successful in managing an outbreak, this is largely due to a proactive approach to closely monitoring and managing symptoms and suspected cases of Covid-19 and essentially doing everything possible to stop it in its tracks.
Contact tracing
It is advised that carers should only work in one home while this pandemic is still ongoing and daily temperature checks should be carried out. All contact should be treated as close contact during the pandemic, and staff should be supported if they need to isolate after contact with a confirmed Covid case. Care facilities need to emphasise that staff will not be penalised and should not come to work when they are not feeling 100% even if there is a staff shortage. All care workers should be encouraged to report if they are feeling unwell and remain at home if they are showing symptoms. Testing should be arranged for these members of staff – there is now a government service dedicated to conduct testing in care homes (https://www.gov.uk/apply-coronavirus-test-care-home) which in time is expected to allow everyone in a care home to be tested.
Strict isolation policies
Carers should be segregated and only work with either suspected/confirmed residents with Covid-19, or those who are not infected and have clear signage as to who is in isolation and who is not.
There needs to be a strict isolation policy for anyone showing symptoms or suspected to have symptoms, including 14 day isolation for anyone being transferred from another home or facility, plus testing for these residents where possible. Residents who are isolating should do so even for meal times and all non-essential travel outside the home should be cancelled. Care teams must ensure all immunizations are up to date.
Be aware of potential asymptomatic residents
If transmission in a care home is suspected, then testing those who have potentially come into contact with the virus could highlight asymptomatic patients who would have otherwise gone undetected, thus causing a larger outbreak and more potential fatalities.
How Nourish is helping care homes to closely monitor and manage the spread of Covid-19
At Nourish, we have created digital protocols for managing Covid-19 across care teams and people receiving care and support: our Covid-19 Trackerallows care homes to record, track and monitor symptoms and cases of Coronavirus within each care team.
The protocol includes:
Nourish has also launched a free version of a Covid-19 tracker. This tracker can be accessed from any web browser, it’s free of charge, and you do not need to be a Nourish customer to use it. The tracker will allow you to track cases of infections across people in your care as well as your staff by closely monitoring symptoms and other factors. You can record:
Nourish has also been working with the NHS to enable anonymised data to be shared helping towards getting a better understanding of this pandemic across care providers. If you would like to find out more and sign up for the tracker, click here.
In addition to this, during the Covid-19 outbreak, Nourish has also enabled:
For further reading:
Nourish’s Head of Customer Experience, Daniel Hollingworth, talks about the importance of a good night’s sleep, and what can be done to improve your quality of sleep as well as the people you care for.
What keeps you up at night? Perhaps it’s a weak bladder, or the traffic from the street outside. For me it’s more than one cup of coffee a day and a young child who doesn’t seem to need sleep at all.
While the odd bad night’s sleep is normal for many of us, regular disruption to sleep can affect our immune systems, making us more susceptible to illness. Other side effects of poor-quality sleep include sluggishness and slower brain function. This is why monitoring sleep patterns and trends is essential within a care environment, it can help us pinpoint areas for improvement and understand what it is that could be affecting sleep. But how to get better sleep?
Quality sleep is a combination of Rapid Eye Movement (REM sleep) and Non-REM (deep sleep), that allows for rest, rejuvenation and even solidifying memories. REM sleep is also essential for emotional and mental health. Sleep cycles take around 90 minutes, and you ideally want to have at least four of five cycles per night. The average person needs a recommended 7-9 hours of sleep, with the ideal amount sitting around the 8-hour mark.
In a typical care environment, night checks are the norm, and waking state is recorded, and anyone else who appears to be sleeping is recorded as asleep. Although this gives an ok understanding of how much the person has slept or remained awake, it doesn’t actually look at the quality of their sleep.
With a wealth of technology available such as wearables and monitors, we are now able to track sleep quality with great accuracy. When you think of sleep tracking, people tend to think of fitness bands for the wrist, but there are a lot of affordable trackers available, from bedside table noise sensors, under mattress sensors and even wearable rings, these devices can all assess and manage sleep with convenience and comfort.
Everything gets better with a good night’s sleep!
It has been shown that the regularity of your sleep is just as important as the amount of sleep you get at night. It is always better for your health to get regular sleep than to binge on sleep at the weekends, for example. We all feel more alert after a good night’s sleep, but when sleep deprived, the brain has a 40% reduction in capacity to learn.
Research being conducted by Jonathon Cedernaes from Uppsala University in Sweden suggests that sleepless nights can create an increase in an Alzheimer’s related protein called ‘tau’, suggesting a link between poor sleep patterns and more complicated health issues.
Good quality sleep is what boosts our immune system to help fight off disease, so when our sleep is compromised, so is our health. One of the most important factors in ensuring flu vaccines work is to ensure you’re looking after your immune system. Lack of sleep means your body may not be able to create enough antibodies to fight off the virus, therefore resulting in a higher probability of getting flu.
Fortunately, there are many ways we can improve our sleep quality. Many care environments now encourage caffeine free hot drinks, and for good reason. In one study it was found that consuming caffeine six hours prior to bedtime reduces sleep time by one hour. So whether you’re looking to boost your own sleep patterns or wanting to improve sleep in elderly residents you support, a simple change such as switching to decaf can make a difference.
This doesn’t sound that significant until you compare it to further research which found that heart attacks increase by 24% when the clocks go forward in spring at daylight saving time. However, when they go back in autumn, heart attack cases decrease by 21%. This really shows what a difference an hour of sleep can make.
So that swap to decaffeinated drinks really could be a life saver.
Drinking enough fluid is very important and many of the people we support have fluid targets in place for this very reason. Try to drink consistently throughout the day rather than trying to hit your fluid intake in the latter half of the day. The more fluid you drink at the end of the day the more likely you are to make that bathroom trip, breaking your sleep cycle. This also correlates with falls during the night.
Finally, one of the best ways to encourage quality sleep is to increase physical activity. Not only does exercise reduce stress, it has been shown to reset sleep/wake cycles by increasing then decreasing body temperature which triggers tiredness a few hours later.
Better sleep habits and getting good quality sleep is essential in ensuring the body and mind rest, repair and prepare for the next day. Do you monitor your sleep or carry out sleep assessments on those you support to help get better quality sleep in care? Let us know by leaving a comment below
The CQC is starting to recognise the importance of technology within social care and is actively pushing the benefits of a number of technologies such as telecare, telemonitoring, mobile health and digital records. This includes the likes of electronic care planning with a platform such as Nourish. But how a more efficient care management system boost your CQC ratings? .
Going digital is quickly becoming the norm in the care sector and for good reason. Efficiency, data protection and compliance are just a few of the things that make electronic care planning desirable to many care providers. And while they are not currently mandatory within the care sector, they do have a significant chance of boosting your CQC ratings.
What’s wrong with our current way of working?
Nothing. Many care organisations are very happy with their existing structure and processes, but it’s the paper-based system that’s slowing them down. There are plenty of organisations who have good or outstanding CQC ratings even with a paper-based system, but an electronic care planning system can help you achieve these scores quicker and easier, so you can actually focus on giving person-centred care rather than feeling like you’re always filling out paperwork purely to meet CQC’s expectations.
Having everything recorded in one place can make audits far less stressful, and as the CQC also start to realise how much easier it is to complete an inspection when everything is managed electronically, making the switch to a digital way of working seems the natural way forward.
But electronic care planning isn’t about changing the way you work, it’s simply about using a different platform to enhance your current way of working. At Nourish we designed a totally flexible platform that can be moulded to suit your current way of working, not the other way around, while allowing you to reap the communication and responsiveness benefits of managing information digitally.
No matter what type of care you are providing, whether it be residential care for older people, support for people with learning difficulties, mental health, dementia or other, Nourish’s electronic care planning system can help you focus on the people you support rather than paperwork.
Isn’t it just the same as what we do now, but on a computer?
Electronic care planning can be so much more than what it says on the tin. Some electronic care plans are quite literally just digitally recorded care plans, the same as they are on paper. While these do have some benefits, in order to see changes in efficiency, you need a platform that is going to refine the way you already do things, so that it’s quicker, easier and clearer for carers to use.
In order to use electronic care planning to improve your CQC ratings, you don’t necessarily need to change the way you provide the care, only the way you record and evidence it. Electronic care planning can offer different ways of doing things that allow you to stay focused on person-centred care, most importantly, it can allow you to have more face-to-face time with those you support rather than spending time on lengthy paperwork.
Nourish is an innovative platform with ever-evolving features that can help you provide better daily care outside of the electronic care plans. So whether you already have an effective structure in place or you’re looking to improve the way you do things, Nourish’s electronic care planning system has a lot to offer.
Transparency of Care is Key
We believe transparency and consistency across care teams is essential when it comes to achieving good and outstanding CQC ratings. Nourish is designed in a way to encourage clearer communication to empower carers across the sector.
We want to help you provide the best quality care in the simplest form. Rather than try to create something very complex, we have kept the user interface clutter free and the features limited to the things you need. Care plans are one of our most-used features, however there are many other features which have proven to be incredibly useful when it comes to meeting CQC standards.
How electronic care planning can help
Nourish has a number of unique features that can help you build a more effective care management system and boost your CQC ratings. Here’s just a few…
Seamless handovers
Nourish’s handover feature is one of the main ways we encourage transparency across care teams. If one of your members of staff comes back after a week or two of holiday, catching up can seem impossible with a huge pile of papers to work through. This is where things can get missed and your CQC ratings could slip.
The handover feature allows you to view the past days and weeks all in one place, and easily pick out any important notes that may have been recorded in your absence. Carers can leave specific handover notes for those who are absent, and these are then there for when they come back to work. It’s also the perfect tool for ensuring everyone knows what’s happening at the changeover of shifts, so someone starting the night shift will be able to clearly see everything that’s happened throughout the day.
These notes will also be visible in the relevant sections and can be viewed when recording at the point of care and can also be read easily by a CQC inspector and evidences the clear communication within the team
Body maps
Skin conditions are usually monitored and recorded on paper, which means that when changes occur (which they can do frequently), it can be difficult to update the records quickly enough to pass this information on to a wider team. The body map feature allows you to report on new and existing skin conditions at the point of care, creating a clearer flow of communication and reduces the risk of mishandling of those who do have certain conditions.
The transparency that this feature ensures that everyone is equipped with the relevant information to do their job safely and effectively, and with everything recorded on the body map within the Nourish app, when it comes to a CQC inspection, there is clear evidence of how you manage this.
Scored assessments
Nourish’s scored assessment feature allows you to closely monitor those you’re supporting in order to provide the right kind of care. By answering a series of questions, Nourish can then generate a score and create alerts for certain things so that carers can react quickly to change.
This provides a more accurate way of tracking things such as nutrition, fluid intake, behaviour, wellbeing and more, so that you can provide care that is completely tailored to the individual’s needs.
With a slicker, smoother way of creating care plans, recording notes, and managing staff, everyone benefits from electronic care planning. Not only are people receiving more person-centred care, but carers feel empowered by the open communication and clarity surrounding care plans, which ultimately makes for far more efficient management within the care sector.
No matter what your current CQC rating, the Nourish system can help you improve your overall efficiency, saving you time and stress when it comes to those all-important CQC inspections.
Those details that make your care team stand out and life more colourful
When care teams have the right culture and values and the time to focus on each person, this becomes visible in the little details: receiving personal care according to the individual’s preferences, finding what is meaningful for each person and enabling each and every one to have aspirations.
Whether that’s watching the cricket, feeding the ducks or checking the grandson’s new update on Facebook. Being able to demonstrate how your team goes above and beyond to help each person they support find meaning and wellbeing every day is a big part of what moves the needle towards the coveted Outstanding rating.
And Nourish enables exactly that do be done simply, by configuring each interaction so it’s aligned with personal preferences, or by recording ad-hoc interactions on the go, with photos, voice annotations recorded by your team or the person themselves. It’s the ultimate demonstration that each person is living a fulfilled life, above and beyond being kept safe, their life has meaning, and the care team is able to innovate every day to improve the wellbeing of those they support.
Moving away from what we know and stepping into the unknown can be a daunting experience. For both businesses and individuals, change isn’t easy and is often something we fear given it isn’t something that comes naturally; but should it be or should we actually fear just standing still? . In the words of Susan Jeffers sometimes we just need to ‘Feel the Fear and Do It Anyway’. This is particularly true when it comes to using digital in social care.
This notion of change and not being fearful of it is something that our founder and CEO, Nuno Almeida, touched upon at this year’s Care Show. Representing the ‘Care Software Providers Association’ (CASPA), Nuno addressed the issue of change in relation to the use of digital technology within the care sector.
Although more and more care services are adopting the use of digital technology, there is still an enigma that surrounds the evolution of it within the care sector. It’s hard to believe that in the UK, over 75% of care providers still use a pen and paper for planning and record keeping, rather than using electronic care planning systems. Whilst the care sector has evolved over the years, changes have been slow. There are still a lot of fears associated with digitalisation and its perceived risks. Key concerns revolve around:
All valid and understandable reasons as to why care providers are cautious of changing to a digital way of working. However, as Nuno raised the point, could paper present a bigger risk?
Records can be lost; information can be hard to find, and it can be hard to provide carers with context in terms of what is needed for those they are supporting. In the main paper records are seen more as a statutory obligation. A log of evidence to show standards of care to the likes of CQC and local authorities. The data isn’t being used in a way that can help us to improve and enhance care, something that digital technology can help overcome.
When records are input into a digital system, they become so much more than just evidence for inspection. They open up a whole new world of possibilities that simply wouldn’t be possible with stacks of paper. For example using an electronic care planning system to record digital records enables:
Clearly digital technology such as electronic care planning can provide care providers with a range of benefits, but how can the fear of change be overcome? Like with most things, when you are armed with the right information and the right guidance, change becomes less like something that should be feared and more like something that is manageable and exciting.
In Nuno’s words ‘with the right co-ordination, the right strategy and the right partners, we can get the right digital use in social care’ and this is one of the key aims of CASPA. To help promote and continue to grow the use of digital technologies in the social care sector to improve the quality of care delivered.
To ensure a smooth transition, there are a number of actions care providers can put into place to help when moving to electronic care planning. CASPA suggest the following guidance on how to source and implement digital transformation software.
So you’ve chosen the provider you want to use, but what next? Well you will need to consider how you will implement the new digital system. CASPA suggest following a three-step process for implementation:
Ensure you communicate with families and care teams in a way that is reassuring and clear about the reasons for adopting digital. Try to build excitement and show that this change is positive and something that they don’t need to be nervous about.
Agree whether your chosen supplier will train all your staff or just your internal training team who will then deliver the training to the remaining members of your staff. Once this has been agreed deliver your training accordingly. Give your team reassurance that they can tackle and deal with the change and help them to feel in control by showing them that there are clear plans in place for training and roll-out.
Agree how devices are prepared and deployed. Tell staff where they need to be and when. Ensure you know how user accounts are created and how records are created for the people you support.
Good providers will be able to provide you with all the information you and your team need to ensure you are comfortable and ready for the transition to digital. From giving you clear guidance about GDPR responsibilities to how to manage devices and lock them down should they go missing. When looking for a provider CASPA recommends asking the following questions to help you find out whether they would be a good fit for you:
About the Care Software Providers Association (CASPA)…
CASPA has been established in the UK as an independent, not for profit, member-driven association. The association is currently led by a volunteer group of founding board members, each of whom manages a well-established software company that provides solutions for social care providers
CASPA Mission…
Find out more about whether using an electronic care planning could help you and those you support here.
Care providers far and wide are already making the transition to digital care management; benefiting from higher quality care plans and notes, compliant and accurate audit trails and a greater degree of control across the management process.
These benefits are being felt at every level, from care managers and carers to the people they care for and their families. Here, we talk to three experienced care providers about the individual impact Nourish Care is having across the entire care service.
For carers, Nourish is empowerment at the point of care. By using well designed and easy to use applications on handheld devices, carers can record notes as they go.
Carers are thereby able to focus a lot more on the person they are working with, and encouraged to record the person-centred care notes that inspectors say distinguishes a care service. Recording notes alongside care also promotes greater clarity, adds useful context and ensures all information is recorded as soon as possible – not forgotten over the course of the day. Recording as they go, carers have the opportunity to really demonstrate the great quality of care they are giving.
Simon Francis, IT Project Manager at Silverline Care, commented: “The main thing for our carers is that the recording of notes is a lot easier. What they were doing beforehand was having to provide care and then try and hold all that information until the end of the shift. Care for residents is now much more to the point and accessible. There is better communication between staff and everyone involved in the client’s care can see what care has already been provided by others. This has made handover a lot easier. It also means input from the carers feeds directly into the care plan, meaning it’s updated within minutes of it taking place. Recording in real time means we don’t lose any important information.”
Paul Dennis-Andrews, Operations Manager at Encompass, has been working with the Nourish Care since spring 2016. He added: “The digital care management system has had a highly positive impact on the overall culture of our service – more than we ever would have thought. Staff who might have had difficulties with the written word are enthused by the ability to speak verbally into the devices to record information. It has been a refreshing and efficient change to a longstanding process of handwritten documentation.
“The large collection of paper files has been replaced with discrete modern handsets and tablets that staff can keep on their person, promoting highly person-centred support exactly how the individual would like to receive it. Documentation is recorded live and visible immediately to anyone with permission, and every aspect of the system is customisable and can be evolved to needs.”
Probably one of the biggest benefits for senior carers and care managers is that all information is in one place and accessible at any time. Care notes and assessments feed directly into the care plans and can be accessed by all who need to see them. This develops a culture of knowledge-sharing and allows for more effective care monitoring and visibility of critical information in real-time.
Digital care management also allows for instant reporting, which gives managers back their time to ‘walk the floor’ and interact with their staff and clients.
Megan Read, Care Home Manager of Grassington House emphasises how the digital system has improved her ability to manage: “Because I have a digital overview of real-time information I can easily monitor what is happening within the home. I can set up anything I want to be recorded, schedule things for the carers to be aware of and make sure that nothing is getting missed.
“For when I’m conducting care plan reviews, I can look at the logs that carers input to directly review and evidence any changes made. Beforehand, you would have had to look through endless files and pages, and you simply wouldn’t be able to go through it all. Now, I have no files in the office, everything is on the system; my office can literally move around with me anywhere.”
Simon agreed: “In leadership, the digital system is allowing managers to spot issues more quickly; alerts raised by carers come straight through to the manager, who can then respond quickly and with all the necessary information”.
Paul added: “Monitoring the quality of the support provided is much more efficient and less intrusive; utilising the Cloud to view live records. It is easier to ensure care is being given and support is provided how the individual would like to receive it. Teams are now positively communicating and sharing ideas, and where changes are required, managers can make these instantly, either across the organisation or simply for individual.”
Managers can also easily establish what information they want recorded, and monitor whether this is being followed. Megan states: “As a manager I can literally prompt what information I want recorded from carers and when. The amount of detail I can now see in recorded notes is amazing compared to what it used to be on paper.”
Simon has also experienced improved quality of care information: “During the transfer to digital care management, we’ve been able to see the quality of our care plans. It is an impossible feat to trail through reams of paper plans for every single resident, but with digital we can check care plans easily and demand the quality we want. It’s meant we can really see the overall process and make sure the right care is being delivered in line with the residents wishes.”
As Simon and Paul state, by recording care as you go, you create a more person-centred and accessible quality of care and you have more time available. Carers have the tools and information they need to provide personal and responsive care, and with extra time, can involve the resident directly and sociably in inputting the care notes.
Megan encourages her carers to be sociable and engage the residents when writing notes; this can mean sitting down with the resident, having a cup of tea and a real conversation about how the resident is doing. She has found that residents prefer the digital care management system once they understand it because carers are able to spend more time with them. Megan commented: “Carers can be sociable and engage with residents so they can contribute to their own notes, keeping them much more involved with their care. Beforehand, carers would have to spend time away from the residents at the end of the shift completing paperwork. The digital system is also really useful for bi-annual reviews; I can hold a meeting in the lounge and connect my laptop to the main screen so we can all see the information and have a really good chat about the care plan with the resident – it’s a lot more involved, but also efficient, and residents like to be able to see their care plans so easily.”
Care information recorded electronically is also much easier to share; not only with other medical professionals, but also with close friends and family. Innovative care providers can utilise existing resources and involve these other parties from the very beginning; you can enable a service user to design their own care plan, involve family members in the on-boarding process or allow informal carers to contribute directly to the care notes. Having a digital system opens up vast opportunities to get better connected with the whole circle of care.
By enabling better communication and ensuring information is shared with those who need to know, your care team will be more aware of the individual service user’s needs; and ultimately, informed care leads to better care.
Get in touch today to see how digital care management can work for you.